
If you’re reading this, you probably know that Lisa is gone.
On October 19, four months after the day she died, we gathered with a small group of family and friends to dedicate a bench to her memory in a beautiful spot not far from our home. It was a looser, smaller, less formal occasion than her funeral in June. We called it “the Benchwarming.” We did everything we could not to plan it. People spoke, hugged, laughed, cried. “The Historian” (that’s me) brought his guitar and sang “The Rainbow Connection,” at Lisa’s non-negotiable request. “The Prophet” bravely and beautifully read the poem “When I Am Among The Trees,” by Mary Oliver, a favorite of Lisa’s and the source of the line on her bench’s commemorative plaque. And “La Neige” read her own eulogy, posted below, with exquisite poise. (The eulogies from the funeral are posted here.)
When I Am Among The Trees
(by Mary Oliver)
When I am among the trees,
especially the willows and the honey locust,
equally the beech, the oaks and the pines,
they give off such hints of gladness.
I would almost say that they save me, and daily.
I am so distant from the hope of myself,
in which I have goodness, and discernment,
and never hurry through the world
but walk slowly, and bow often.
Around me the trees stir in their leaves
and call out, “Stay awhile.”
The light flows from their branches.
And they call again, “It’s simple,” they say,
“and you too have come
into the world to do this, to go easy, to be filled
with light, and to shine.”
La Neige’s Eulogy
It is impossible to describe a life in one single speech—or even in one hundred speeches. Especially not when the person in question is the most amazing person you have ever known.
Instead, I would like to thank everyone who has come here today to remember my mom. It was one of her requests that we dedicate a bench to her in a park we visited frequently.
Mom loved nature, and she especially loved helping out. Something she enjoyed taking part of was Interfaith Tree Planting. If you haven’t heard of it, it’s an event where the Jewish community, the Christian community, and the Muslim community come together to plant trees. Whenever we did it, we’d more often than not end up covered in mud and smelling like dirt, but it was always worth it. Mom was a huge supporter of Interfaith Tree Planting, and even helped plan it when she was on our synagogue’s Social Action Committee. Even after she was diagnosed with cancer, even when she wasn’t feeling great, she would still come and help plant trees.
Mom had a green thumb, too. She would grow beautiful flowers, which she would then cut and place in vases around the house. She was always giving flowers to others, too, for them to put on their own dining room tables presumably. She had a great eye for which flowers would look best in our window boxes and on either side of our porch stairs. When we renovated our back yard, Mom made sure that we planted lots of new plants—everything from ferns to Japanese maples. We named all of the trees we planted, and the ferns, too.
And then of course there were our nature walks. We’ve been doing them for as long as I can remember. We’ve gone to so many different trails, with many different people. But we’ve always gone as a family. We’d drive out to a beautiful location, often a forest, and we’d just… walk, together. Sometimes we talked. Mostly we would just walk in silence, each of us lost in our own thoughts, each of us finding our own things to admire and appreciate in the world around us. To me, this was always one of those special times when you truly feel at peace. We’d walk in the warm summer and the cold winter, and of course the beautiful spring and fall in between. Nature walks are some of my fondest memories—they were the times when I felt the most connected, both to Mom and to the world around me.
Mom believed that there was beauty everywhere, and she was constantly encouraging us to stop and see it too. She knew better than anyone that life isn’t always beautiful, but she still found small things to point out to us—things that I never would have noticed on my own. Even when the colours of the falling leaves weren’t quite at their peak, she would still appreciate them regardless. She could always find something to admire in the world around her.
And more often than not, her enthusiasm was contagious. She made me see the world with different eyes, and notice things that I wouldn’t have noticed otherwise: those pretty flowers in a neighbour’s garden, that unique bird call that I’d never heard before, or the way the leaves crunched beneath my feet.
Mom, I miss you every day. I think that everyone here does. But I also see you everywhere in the world around me—in the bushy-tailed squirrels, in the vibrant autumn foliage, and especially, in the trees.
Thank you.






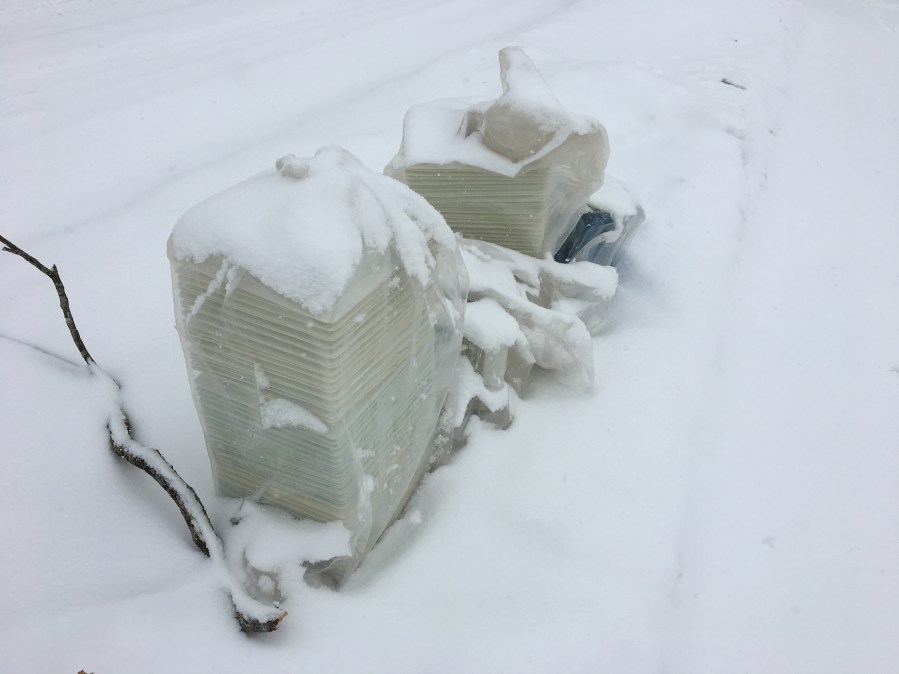




![IMG_0818[1]](https://breathinginbreathingout.blog/wp-content/uploads/2018/12/IMG_08181.jpg?w=640)